PGY 1
In the first year, interns build a strong knowledge base and the foundation of critical skills related to the assessment and management of the acutely ill patient.
Orientation 2 weeks
UMC ED 25 weeks
Community ED 2 weeks
Rural ED 2 weeks
Peds ED 4 weeks
MICU 4 weeks
CCU 2 weeks
OB 2 weeks
Anesthesia & US 2 weeks
Subspecialty 2 weeks
Selective 2 weeks
Vacation 3 weeks
PGY 2
In the second year, residents complete several ICU rotations where they learn to manage the critically ill and medically complex patient. They also take ownership of ED patients including running Traumas, Codes and all ED airways.
Admin 2 weeks
UMC ED 18 weeks
Community ED 4 weeks
Rural ED 2 weeks
Peds ED 4 weeks
Psyc ED/ US 2 weeks
TICU 4 weeks
MICU 4 weeks
Tox/QI 2 Weeks
EMS 2 weeks
Selective 2 weeks
Elective 2 weeks
Vacation 4 weeks
PGY 3
Third year residents function as “Charge Residents” where they take the lead role managing students, junior residents and an entire patient care area.
Admin 2 weeks
UMC ED 20 weeks
Community ED 4 weeks
Rural ED 2 weeks
Peds ED 4 weeks
MICU 4 weeks
PICU 4 weeks
Tox /US 2 weeks
Burn Unit 2 weeks
Selective 2 weeks
Elective 2 weeks
Vacation 4 weeks
PGY 4
Senior residents are granted ample flexibility during their fourth year to further develop their niche interests or continue a subspecialty track.
Admin 2 weeks
UMC ED 18 weeks
Community ED 8 weeks
Rural ED 2 weeks
Peds ED 4 weeks
Teaching 2 weeks
Selective 4 weeks
Elective 8 weeks
Vacation 4 weeks
Program
Unique Features of Our Residency
In order to develop well-rounded physicians, our program incorporates graduated responsibility, near-peer teaching, and the social determinants of health.

Charge Resident System
The Charge Resident System is based on a model of graduated responsibility and constitutes a core value of our educational philosophy to develop excellence in leadership, education, and professionalism.
The Charge Resident is ultimately responsible for supervising patient care and determining all medical decision making for a 14-bed section of the ED. They oversee a team of interns and medical students, take clinical presentations, prioritize and delegate tasks, supervise all procedures, conduct shift change rounds and manage patient flow. In the Trauma Bay, the Charge Residents leads all resuscitations and manages the airway for all trauma patients. Additionally, they serve as medical control and respond to all radio communication from EMS regarding medical treatment questions, transport decisions, and trauma activations.
Upon graduation, our residents have significant experience navigating operational challenges, managing departmental flow, and caring for medically complex and critically ill-patients while continuing to provide superb patient care.
Social Emergency Medicine
The Social Emergency Medicine curriculum allows residents to further investigate the social determinants of health and how they impact patient care. Our program is a pioneer in the development of this subspecialty and our residents and faculty hold a wide range of local, state and national leadership positions in the field. This integrated curriculum involves site visits to local clinics, completing online training modules, engaging in community activities, and participating in advocacy on a state and national level. All residents are required to complete the basic curriculum and for those who have a vested interest in the area, a dedicated elective and sub-specialty track is available.
Rural Emergency Medicine
Lallie Kemp Regional Medical Center is a critical access hospital located 90 minutes outside of New Orleans in Independence, Louisiana. Residents spend two weeks annually rotating at Lallie Kemp where they gain experience making clinical decisions in a rural environment without access to sub-speciality services. Residents learn to become self-reliant and master the ability to rapidly stabilize, treat and transfer the acutely sick and injured patient. Our residents enjoy working at Lallie Kemp so much that many of them choose to moonlight there later in residency.
Residents as Educators
Our residents have a tremendous opportunity to develop their skills as educators throughout their training and regularly participate in an array of teaching activities for a variety of learners. Our Emergency Department at UMC serves as the dedicated teaching hospital for both Tulane and LSU Medical Schools and our residents oversee nearly 400 rotating medical students annually. In addition, we are the primary training site for LSU’s PA and nursing students as well as the United States Navy SEAL medics. Furthermore, our residents serve as educators in the following programs:
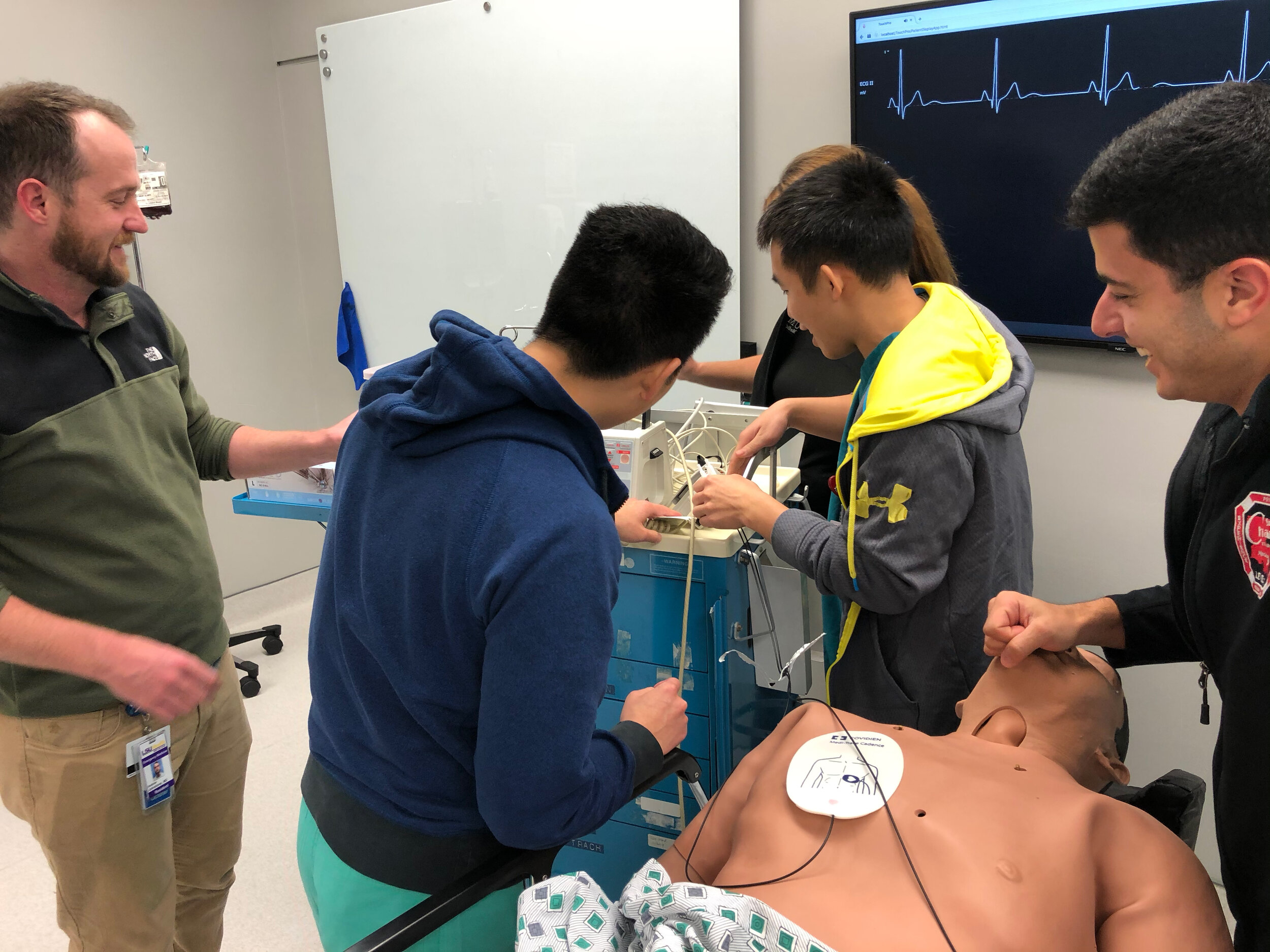
Simulation, Ultrasound, Procedure & Cadaver Lab Instructors
ACLS Instructors
Stop the Bleed Instructors
“Big Buddy” Mentorship Program for medical students
Foundations of Emergency Medicine Course Instructors
Dedicated 2-week Teaching Rotation
Lectures during weekly educational conference
Elective/Selective Time
Our residents are granted a total of 22 weeks of Elective and Selective time in order to explore the sub-specialties within Emergency Medicine and ultimately develop a niche for their career. Residents may purse any pre-approved elective of their choosing or can design their own elective opportunity. For Selectives, residents may choose from rotations such as: Palliative Care, Pain Management, Physical Medicine & Rehabilitation, Radiology, Oral Surgery, Dermatology, ENT, Administration, Informatics, Simulation and others.





